In the midst of this pandemic, during September 1918, cities around the US were planning parades to promote liberty bonds, being sold to help pay for the war effort in Europe. In Philadelphia, Pennsylvania, where 600 soldiers were already infected with the flu virus, city chiefs decided to go ahead with their parade. Meanwhile, the city of Saint Louis, Missouri, opted to cancel their parade and introduce other measures to limit public gatherings. One month later, more than 10,000 people in Philadelphia had died of Spanish flu, while the number of fatalities in Saint Louis stayed below 700.
The parade was not the only reason for the difference in death rates, but the figures show the importance of measures now known as “social distancing” can have during pandemics. “Social distancing refers to a way of creating a barrier of physical distance between two or more people so that transmission of virus can be prevented or halted,” says Arindam Basu, associate professor of epidemiology and environmental health at the University of Canterbury, in New Zealand.
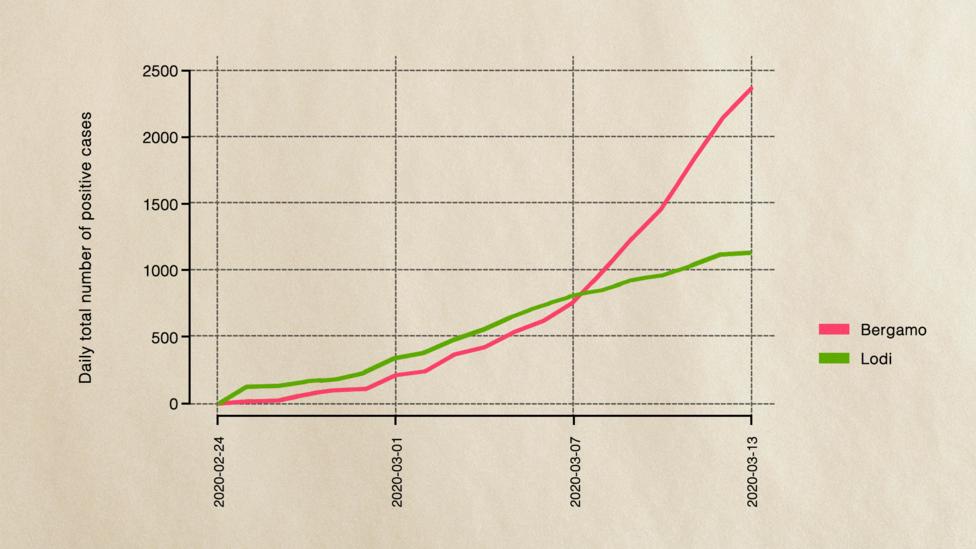
One analysis of the interventions made in several cities around the US during 1918 showed that those that banned public gatherings, closed theatres, schools and churches early had far lower peak death rates.Just over 100 years later, the world is facing another pandemic, this time from a different virus – the Covid-19 coronavirus. Today the global population stands six billion higher than it did in 1918. While Covid-19 is different in many ways from the Spanish flu – particularly in terms of who it affects and its mortality rate so far – there is a very important lesson about the difference social distancing can make. It might still be one of the best ways of fighting this pandemic. (Read more about the other lessons we can learn from Spanish flu.)
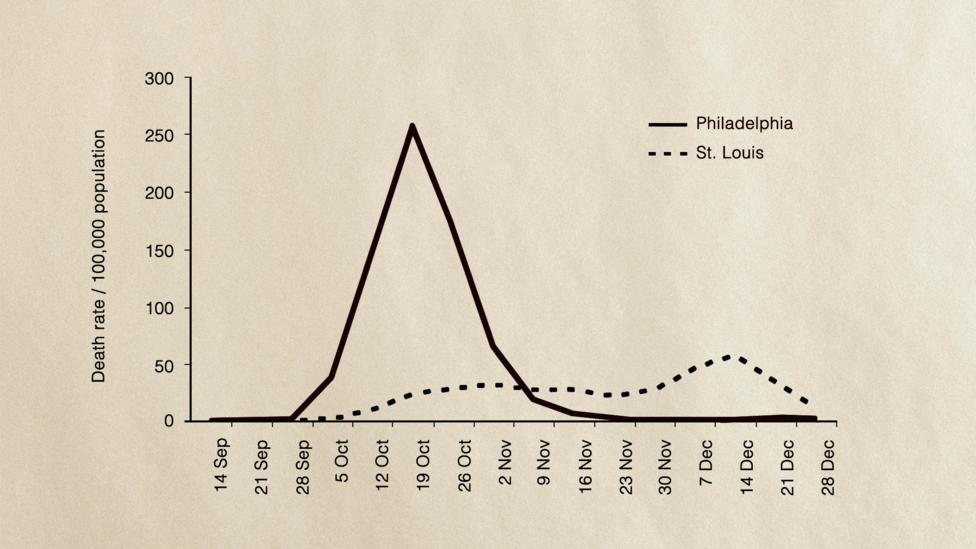
The death rates in Philadelphia and St Louis during the 1918 Spanish flu pandemic demonstrate the importance of social distancing (Credit: National Academy of Sciences USA 2007)
“At this time, we do not know of a safe and effective vaccine, nor do we know if a safe and effective drug will work to eliminate the Covid-19 infection once it has occurred,” says Basu. “In the absence of these, our best bet is based on prevention.”
Many countries around the world are now experiencing different measures in an attempt to enforce social distancing to slow the spread of Covid-19. They range from ending mass gatherings, closing public spaces like leisure centres, pubs and clubs to closing schools and in some places a total lockdown with people forced to stay indoors.
While self-isolation is a form of social distancing, there is an important distinction to be made. Self-isolation and quarantine are aimed at preventing people who are infected or are known to have had contact with people who are infected from passing on the virus. Social distancing is a wider measure aimed at stopping the kind of mixing of people that allows infections to spread through a population. (Read more about what social distancing means.)
And we may need to keep our distance from others for some time to come. New computer modelling research from Harvard University, which has yet to be published in an academic journal, warns that it may be necessary for intermittent social distancing measures to be maintained into 2022 in the US unless other interventions such as vaccines, drug therapies and aggressive quarantine measures can be put into place. This is because while a one-off period of social distancing might delay the peak of the outbreak until later this year, there is likely to be a resurgence in cases towards the end of the year if the virus shows some seasonal variation. (Read more about how Covid-19 might change with the seasons.)
But there is a good reason why social distancing has become such an important strategy in controlling the Covid-19 pandemic.
Each person infected with the Covid-19 coronavirus is thought to pass it on to an average of 2-3 other people in the early stages of an outbreak. This contagiousness is measured by epidemiologists using something known as a “reproduction number”. By comparison, influenza has a reproduction number of 1.06-3.4 depending on the strain. Spanish flu was found to have a reproduction number of about 1.8 by one study. Rhinovirus, which is one of those that causes the common cold, has a reproduction number of 1.2-1.83. Most estimates for Covid-19 have put its reproduction number at between 1.4-3.9.
Watch
 info@businessghana.com
info@businessghana.com